Conference Posters
These conference posters are preliminary reports of work.
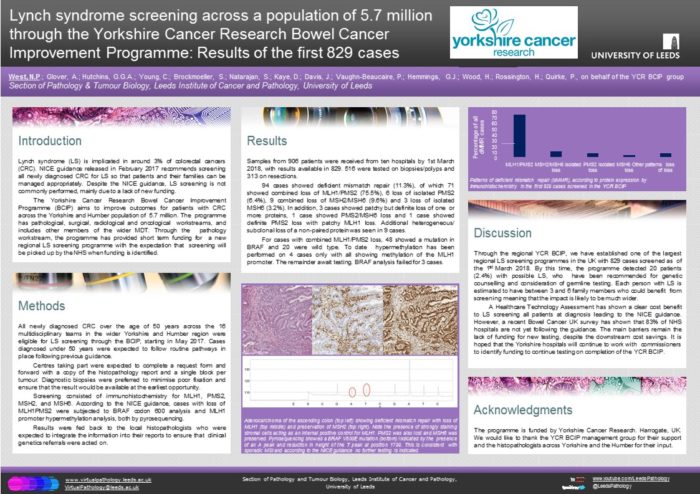
Lynch screening across a population of 5.7 million through the Yorkshire Cancer Research Bowel Cancer Improvement Programme: Results of the first 829 cases
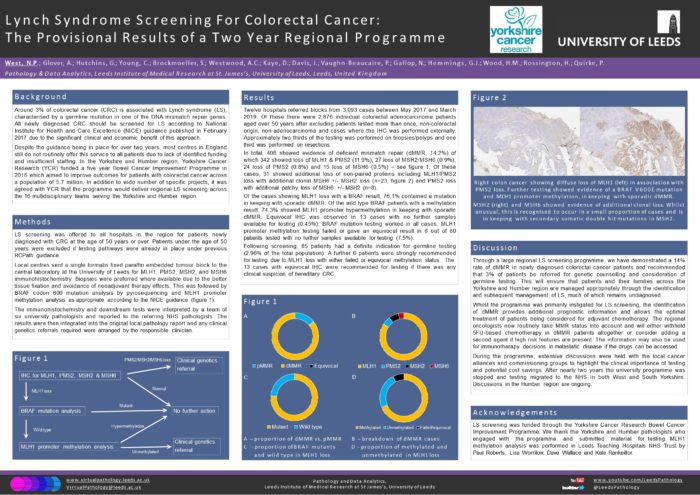
Lynch Syndrome screening for colorectal cancer: the provisional results of a two year regional programme
Presented at Leeds Pathology 2019.
Abstract:
Around 3% of colorectal cancer (CRC) is associated with Lynch syndrome (LS). All newly diagnosed CRC should be screened for LS according to NICE guidance yet most centres do not routinely offer this service due to lack of identified funding. Here we report the two year results of a regional LS screening programme offered to 16 multidisciplinary teams serving a population of 5.7 million.
Screening was available for all patients diagnosed with CRC over the age of 50 years. Local centres were asked to refer a formalin fixed paraffin embedded tumour block (preferably biopsy) to the central laboratory for MLH1, PMS2, MSH2, and MSH6 immunohistochemistry. This was followed by BRAF codon 600 pyrosequencing and MLH1 promoter methylation analysis as appropriate.
Twelve hospitals referred blocks from 2415 patients between May 2017 and March 2019 (66% biopsies/polyps and 34% resections). In total, 335 showed deficient mismatch repair (13.9%) of which 253 showed loss of MLH1/PMS2 (10.5%), 20 loss of MSH2/MSH6 (0.83%), 15 loss of isolated PMS2 (0.62%) and 13 loss of isolated MSH6 (0.54%). In addition, less common combinations of protein loss were observed in 34 cases (1.4%). Of the cases showing MLH1 loss, 75.5% contained a BRAF mutation. Of the wild type BRAF patients, 82.3% showed MLH1 promoter hypermethylation.
Following screening, 68 patients were strongly recommended for LS germline testing (2.8%).
Through a large regional LS screening programme, we have demonstrated a 14% rate of deficient mismatch repair and recommended 3% of patients to be referred for genetic counselling and consideration of germline testing. This will ensure that patients and their families are managed appropriately with regard to adjuvant chemotherapy decisions and the identification and subsequent management of LS.
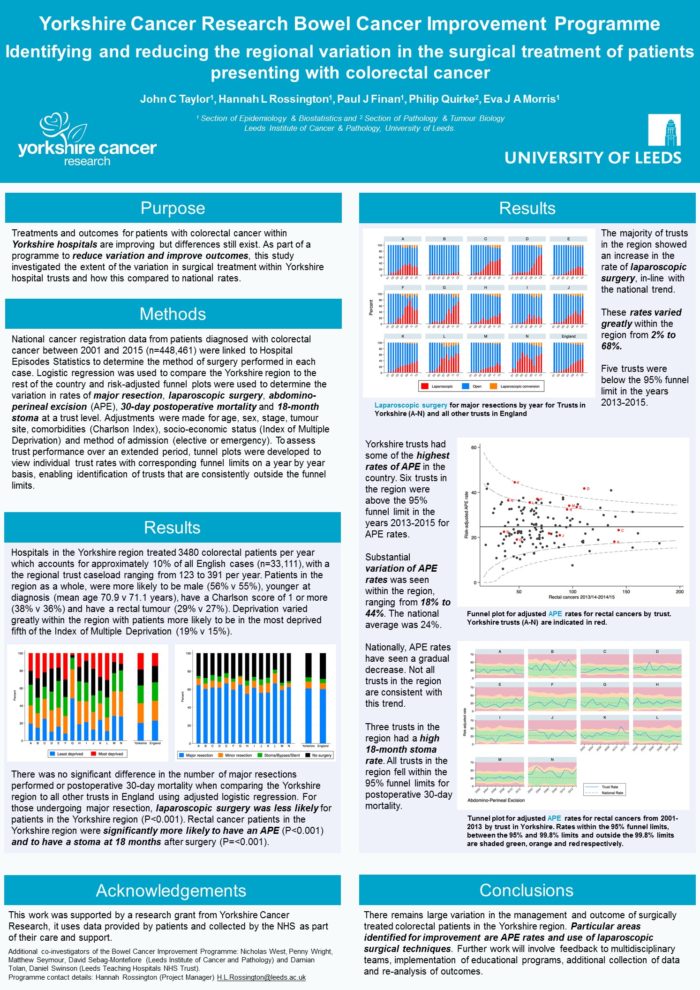
Identifying and reducing the regional variation in the surgical treatment of patients presenting with colorectal cancer
Presented at The Association of Coloproctology of Great Britain and Ireland 2017 Annual Meeting.
Abstract:
Purpose - Outcomes, quality and treatments offered for patients with colorectal cancer (CRC) within Yorkshire hospitals are improving but regional differences still exist. As part of a programme to reduce variation and improve outcomes, this study investigated the extent of the variation in surgical treatment within Yorkshire hospital trusts and how this compared to national rates.
Methods - National cancer registration data from patients diagnosed with CRC between 2001 and 2013 (n=379,641) were linked to Hospital Episodes Statistics to determine the method of surgery performed in each case. Logistic regression and risk-adjusted funnel plots were used to determine the variations in treatment and 30-day postoperative mortality rates for Yorkshire trusts.
Results - The proportion of patients undergoing major resection fell nationally but remained relatively high for some Yorkshire trusts, with patients from Yorkshire more likely to undergo major resection (OR=1.12 [1.06-1.19]) compared to no surgery. Within the major resection group, overall abdominoperineal excision (APE) rates were greater in Yorkshire trusts than the national figure (OR=1.19 [1.08-1.32]) with widespread variation observed (18% to 45%). Uptake of laparoscopic surgery for elective cases varied greatly within the region (7% to 65%). Yorkshire trusts mirrored the national picture of a reduction in 30-day postoperative mortality rates but wide variation remained (national 3.5%, Yorkshire 2.4-7.2%).
Conclusions - There remains large variation and scope for improvement in the management and outcome of surgically treated CRC patients in the Yorkshire region. Particular areas identified for improvement are APE rates, use of laparoscopic surgical techniques and factors affecting 30-day postoperative mortality rates.
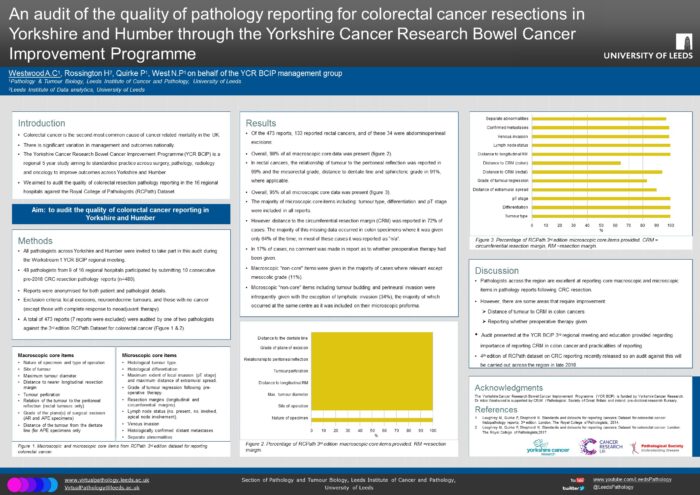
An audit of the quality of pathology reporting for colorectal cancer resections in Yorkshire and Humber through the Yorkshire Cancer Research Bowel Cancer Improvement Programme
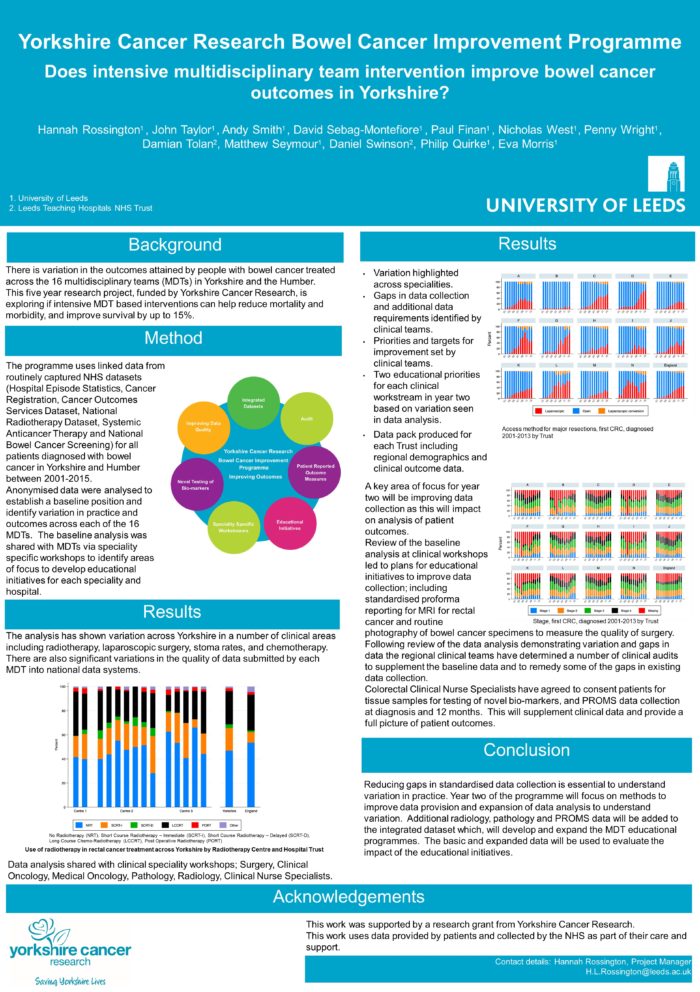
Does intensive multidisciplinary team intervention improve bowel cancer outcomes in Yorkshire?
Presented at PHE Cancer Data and Outcomes Conference 2017.
Abstract:
Background: There is variation in the outcomes attained by people with bowel cancer treated across the 16 multidisciplinary teams (MDTs) in Yorkshire and the Humber. This five year research project, funded by Yorkshire Cancer Research, is exploring if intensive MDT based interventions can help reduce mortality, morbidity and improve survival by up to 15%.
Method- The programme uses linked data through routinely captured NHS datasets (HES, Cancer Registration, Cancer Outcomes Services Dataset, National Radiotherapy Dataset, Systemic Anticancer Therapy and National Bowel Cancer Screening) for all patients diagnosed with bowel cancer in Yorkshire and Humber between 2001-2015. Anonymised data were analysed to establish a baseline position and identify variation in practice and outcomes across each of the 16 MDTs. A quality scoring process was developed to enable measurement of change in improvement in outcomes. The baseline analysis was shared with MDTs via speciality specific workshops to identify areas of focus to develop educational initiatives for each speciality and hospital.
Results- The analysis has shown variation across Yorkshire in a number of clinical areas including radiotherapy, laparoscopic surgery, stoma rates, and chemotherapy. There are also significant variations in the quality of data submitted by each MDT into national data systems. A key area of focus will be improving data collection as this will impact on analysis of patient outcomes. Review of the baseline analysis at clinical workshops led to plans for educational initiatives to improve data collection; including standardised proforma reporting for MRI for rectal cancer and routine photography of bowel cancer specimens to measure the quality of surgery. Colorectal Clinical Nurse Specialists have agreed to consent patients for PROMS data collection at diagnosis and 12 months to supplement clinical data and provide a full picture of patient outcomes.
Conclusion- Reducing gaps in standardised data collection is essential to understand variation in practice. Year two of the programme will focus on methods to improve data provision and expansion of data analysis to understand variation using additional radiology, pathology and PROMS data leading to MDT educational programmes. The basic and expanded data will be used to evaluate the impact of the educational initiatives.
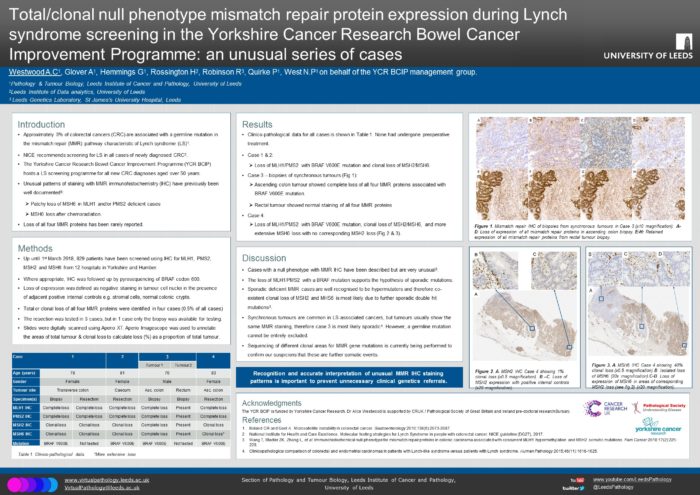
Total/clonal null phenotype mismatch repair protein expression during Lynch syndrome screening in the Yorkshire Cancer Research Bowel Cancer Improvement Programme: an unusual series of cases
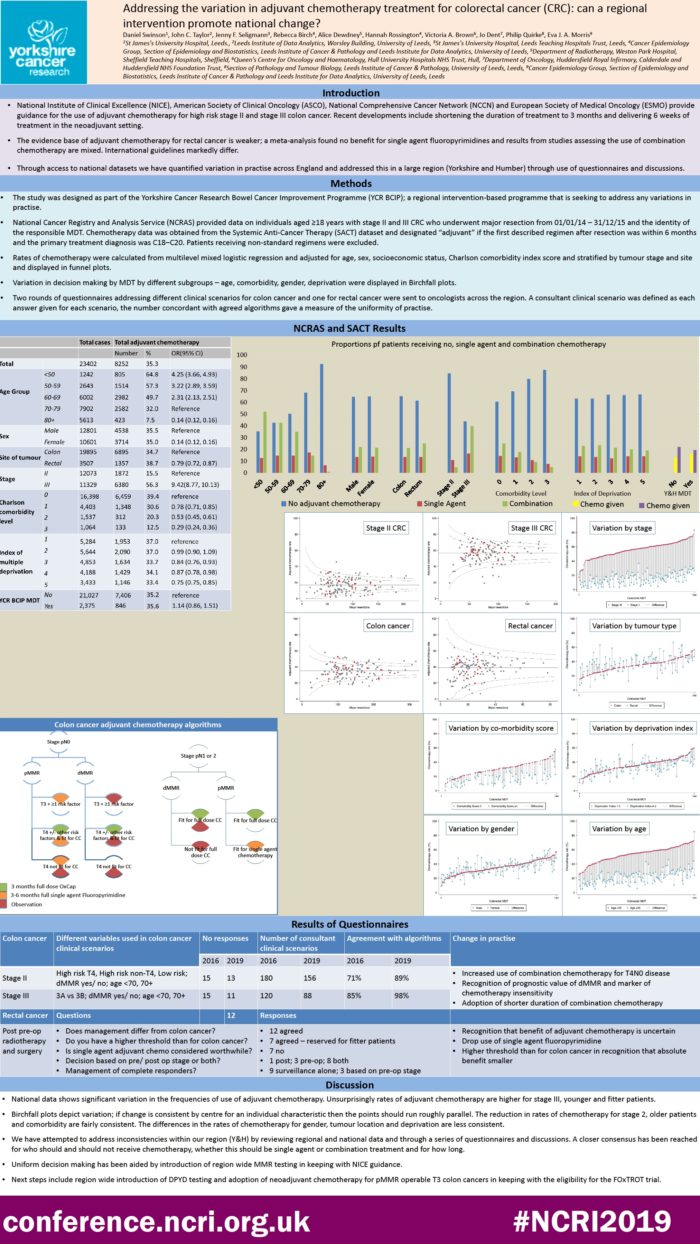
Addressing the variation in adjuvant chemotherapy treatment for colorectal cancer (CRC): can a regional intervention promote national change?
Presented at the NCRI Conference in Glasgow, November 2019.
Abstract:
Introduction:
Analysis of routine population-based data has previously shown that surgery for patients with rectal cancer can vary widely. With access to the Systemic Anti-Cancer Treatment (SACT) database we have quantified variation in adjuvant chemotherapy across England and in detail across a large representative region (Yorkshire and Humber).
Methods:
National Cancer Registry and Analysis Service (NCRAS) provided data on individuals aged ≥18 years with stage II and III CRC who underwent major resection from 01/01/14 – 31/03/16. Chemotherapy data was obtained from the SACT dataset. Rates of chemotherapy were calculated from multilevel mixed logistic regression and adjusted for age, sex, socioeconomic status, Charlson comorbidity index score and stratified by tumour stage and site. A questionnaire addressing different clinical scenarios was sent to oncologists across the region.
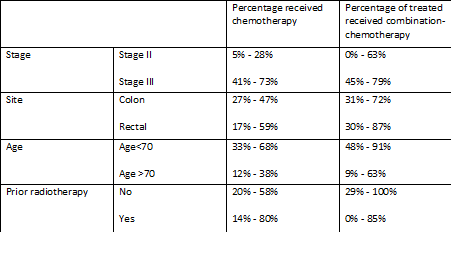
Results:
The national adjusted chemotherapy treatment rate ranged from 2% to 43% & from 19% to 80% for patients with stage II and stage III cancers. Larger variation was seen for rectal than colon cancer, 10% to 70% vs 14% to 60%. Similar variation was seen in region and across subgroups.
A regional questionnaire obtained responses from 15 of 16 MDTs. Widest variation in opinions were for observed for high risk stage II patients both with deficient and proficient mismatch repair tumours and stage IIIB patients over the age of 70.
Conclusion
Variation is seen across England in the use of adjuvant chemotherapy. Open discussion in our region has enabled a consensus agreement on an algorithm for colon cancer, with one pending for rectal cancer.